Welcome. Fungal infection in the eye is rare and difficult to diagnose.
So, here is the first question:
Is your eye tearing, sore, inflamed, red or sensitive to light?If your answer is 'yes', there are several disease conditions which could be causing these symptoms. The more common conditions are allergies, auto-immune reactions and bacterial or viral infections. These conditions are usually easier to diagnose than a fungal infection in the eye.
Read the following questions to see if you are at risk for having a fungal infection in your eye.
Was your eye traumatized in recent weeks, either by an injury to the eye, a foreign body entering your eye, or by eye surgery (such as cataract removal surgery)?
Before your eye became sore and inflamed, were you gardening or working with plant or vegetable matter,compost or wood or was your eye exposed to dust or dirt, even to a gust of wind filled with dust?
Was your eye injured by a possibly contaminated object?
Do you farm or grow crops? Do you handle rotting fruits or vegetables or dirt?
Is your immune system compromised by taking oral steroids, steroid eye drops or by disease or chemotherapy?
This summer, my husband's eye was infected by a fungus.
After several weeks of pain and misdiagnoses, he had to have an emergency corneal repair with a donor patch to save his eye. Because of the fungal infection, he could have lost his entire eye.
Right now, we believe his eye has been saved, but we don't know yet if his sight in the infected eye will recover. He is on strong anti-fungal medication, both oral pills and eye drops.
Fungal infection of the eye is rare and difficult to diagnose.
Many opthalmologists, who aren't specialists in opthamology, have never seen fungal infection of the eye except in text books.
Perhaps our experience can help someone else.
During the time that we didn't know what was causing my husband's eye pain, I found information about eye inflammation on a Blog.
If I had found something about 'fungus' infection of the eye; I probably would have asked for a referral to a specialist sooner. And, maybe my husband wouldn't have needed the corneal patch.
So, maybe this Blog will help someone.
I kept notes of my husband's experience of a serious and rare eye infection caused the Aspergillus fungus:
May 11, 2006 – Elective surgery was done on Ed’s left eye to remove a cataract. A ‘soft’ artificial lens was inserted with no stitches required. ‘Ofloxacin’ eye drops given the day before surgery.
May 12 – Ed’s eye examined post op day one routine check-up. All looks well. Antibiotic is stopped. Prednisolone eye drops prescribed 4 times each day. My husband is healthy and active. He is 70 years old and is not immune compromised. He does not have rheumatoid arthritis (which sometimes causes corneal inflammation).
May 12 – May 26 – Ed has minimal discomfort in his eye. He has lots of energy. Prenisolone drops are slowly being decreased as ordered.
(In hindsight, we believe that, possibly, one day between the 20th and the 25th, Ed's activities caused the Aspergillus spores to enter his eye. We know he clipped the laurel hedge (which required looking up) and did some compost turning. He also worked in the workshop doing woodworking).
We know now that any of these activities could have resulted in the spores of the Aspergillus fungus entering his eye.
For most people, the body's 'protector' cells would have fought off the fungus spores. But, Ed's eye had a traumatized area at the site of the surgical incision for cataract removal.
His eye was also being 'bathed' regularly with Prednisolone drops which inhibit the body's 'protector' cells.
Prednisolone drops are prescribed to reduce inflammation but they also 'mask' infection.
May 27- 28 – 16 and 17 days post operation. Ed’s eye soreness and redness has suddenly increased and his vision has become more blurry. Prednisolone is increased back up to 3 times each day. (our decision due to Ed’s discomfort).
May 29 – Saw eye surgeon for assessment because of Ed’s increased eye redness, light sensitivity and increasing blurred vision and a burning sensation (like acid in the eye). The surgeon can't see anything causing these symptoms and says all is ok, but increases Prednisolone for a few days and starts Ed on Vigamox (antibiotic) four times a day for a week (just in case there is a bacterial infection brewing, according to the surgeon) Prednisolone drops to remain at three times a day and gradually be decreased as per post op instructions.
May 30 - June 9 - Prednisolone and Vigamox are gradually reduced but Ed's eye is still inflamed, painful and Ed is experiencing increasing light sensitivity. I buy him dark, wrap around sunglasses.
June 10 – Ed’s discomfort is still increasing with a pain level of 6 to 8 out of a maximum of 10 for the last 2 days.
He took Tylenol #3 (with codeine) last 2 days but it causes nausea.
He is fatigued easily. The new antibiotic does not seem to be helping.
His eye is still red and it should be healing by now.
He is having increasing light sensitivity and burning.
He is also having ‘shooting pains’ (like needles poking in his eye),
up to 10 times a day.
Sometimes a ‘black shade’ seems to occur over ½ of the affected eye.
Yesterday he felt like a ‘large piece of grit’ was in his eye, but he is not feeling it today.
Two days ago, he felt dizzy and sometimes ‘off balance’ when walking. There has also been a new symptom of ‘clear’ tearing in the last 3 days.
We speak with the surgeon on the phone about Ed's pain, light sensitivity and lack of progress in healing. The surgeon asks if the eye is any redder, and we can only say that it is still as red as it has been.
The surgeon assures us that some people need a longer time to heal from cataract surgery and suggests that we increase the Prednisolone drops back up to three times a day.
June 10-18 - Ed continues to suffer from eye pain. By the 18th, we are very worried and phone the surgeon again, but both doctors are away for a week.
June 19 – We see a doctor in the Emergency Department of our local hospital. She says that Ed’s eye is definitely infected and shows me a yellow ‘square’ on the inner, upper cornea which she says is the site of infection. She encourages us to see an optometrist if we can't see our ophthalmologist. She takes a swab of this raised, dry yellow area for culture and orders CiproFlox (antibiotic) eye drops. Prednisolone to remain at 3 times a day.
June 21 – We see our optomotrist who examines Ed’s eye and says he will immediately 'page' the opthamologist. The optomitrist says that there is a ‘bleb’ in the eye and, although he can't say more about what it might be, he does think the eye should be examined today by the eye surgeon.
The eye surgeon immediately sees us to examine Ed's eye. He says that a piece of the cataract has been ‘missed’, and this is probably causing the eye's inflammation. Apparantly, pieces of the cataract can 'hide' after being broken up during the surgery. Sometimes they absorb over time. This one, it seems, will not. I tell the surgeon what the Emergency room doctor has said about the eye being infected. The surgeon does not believe that the eye is infected; only inflamed.
The surgeon books a second surgery next week to remove the piece of leftover cataract. The Ciproflox drops are discontinued. The surgeon prescribes the Prednisolone drops to be given hourly while Ed is awake. Cyclogel drops twice daily to 'numb' the iris and reduce light sensitivity discomfort. Vigamox drops (antibiotic) 4 times daily.
June 23 – We see a different surgeon for a pre-op exam as this surgeon will be removing the piece of cataract. I ask her about the yellow spot on the inner upper part of the cornea, which the Emergency doctor had said was the site of an infection. The surgeon says that this area is the site of the surgical incision for the first cataract removal and is some form of scar tissue.
We are dismayed about the need for a second surgery but relieved that the pain and inflammation will be eliminated after the surgery.
June 23 – June 26 – Ed is really not feeling well on the 24th due to the eye pain. He has a better day on the 25th when taking Tylenol plain (2 extra strength) every 8 hours.
June 27 – The second eye surgery is performed. The offending piece of cataract is removed. Ed found this surgery very painful as his eye is extremely light sensitive even though his eye is 'numbed' by eye drops during the surgery. He is sent home on Prednisolone and Vigamox drops every 2 hours.
June 28 - Post-op day one routine follow-up by the surgeon.
She says that the surgery was a success but Ed's eye will take some time to ‘calm’ after having the two surgeries. She explains that she put two stitches in this time because it is the second operation. These stitiches can be removed in the office after a few weeks. She explains that her incisions are in different spots from the first surgery. We are to continue on Prednisolone and Vigamox drops every 2 hours.
June 29 – We talk to Ed's first surgeon on the phone and ask about using the Cyclogel drops post-op because Ed’s light sensitivity is highly uncomfortable. He says to use the Cyclogel for comfort and that he wants to see Ed the next day because the long weekend is coming up.
June 30, Friday – The first surgeon says that the eye is still inflamed and will take time to calm. Because of Ed’s eye pain in the nightime (which wakes him up) the surgeon orders a steroid eye ointment to use before sleep. Vigamox drops are reduced to 4 times a day and Prednisolone every 2 hours.
July 1- 3 This ointment does not give relief. Ed’s discomfort remains at the painful level of 3 or 4. Cyclogel drops three times a day for comfort do not seem to help.
July 4 – Examined by first surgeon at routine follow-up. He says that the cornea is improved. The eye pressure is fine. He says that Ed has two choices because of the ongoing pain. One is to carry on as we are doing as the inflammation appears to be slowly reducing. Two is to get a second opinion. We ask what a second opinion might tell us.
The surgeon says that, since the Prednisolone seems to be working, he thinks that a specialist would probably tell us to continue on as we are. We decide to not get a second opinion because of his answer and because it takes up to 3 hours travel to see a specialist. The surgeon stops the antibiotic drops and continues the Cyclogel and Prednisolone drops but not overnight.
July 7 , Friday– The first surgeon has requested this follow-up exam. He says that Ed’s eye has returned to the size that it was before the first surgery and there are only a few white blood cells now in the eye. He says that the eye is healing and wants to see Ed in two weeks. Prednisolone drops are reduced to four times a day.
July 8 – 10 - Ed still must take Advil or Tylenol regularly for pain relief. On the 9th, (Sunday), the pain in his eye reaches a level ‘6’ and wakes him from sleep at 4 am. He has nausea and has to sit up the rest of the night. I am told by a friend about the Eye Care Center, and we decide that we must request a referral as soon as possible. However, we can only see the 2nd surgeon on the 11th (Tuesday). The first surgeon is away.
July 11, Tuesday - Ed's eye is examined by the 2nd surgeon at 10:40 am. She is immediately alarmed and says that the eye is full of white blood cells. She wants us to see a specialist at the Eye Clinic immediately. We go immediately and see two specialists that same day.
July 11 - One specialist tells us that Ed has an infection inside the anterior chamber of his eye and this is extremely serious. He says that Ed’s safety (health) is first and the eye's vision is second. He also asks another specialist to examine Ed’s eye because there seems to be a small hole in the cornea of Ed's eye. We are shocked.
The second specialist (Corneal specialist) examines the eye and confirms a small hole is there as well as a ‘thinning’ or ‘melting’ of the area of the cornea around the hole where the yellow square patch is (the same yellow patch that the Emergency Room doctor had shown to me on June 19).
The corneal specialist ‘glues’ the hole shut and takes samples of the yellow patch and from fluid taken from the eye (with small needles). He is not sure if the eye needs antibiotics injected into it as he is not sure that the problem is a bacterial infection. He puts a clear contact lens on Ed’s eye for comfort.
The specialist says that Ed will probably need a corneal patch graft from a donor after the eye is not so inflamed. He says this graft may cause distortion in vision. Out of the blue, from my place of intuition, I ask if this yellow patch could be a fungus infection? I'm thinking of Ed's Athlete's foot infection between his toes. The specialist cannot tell us at this time until the cultures grow something. We both like the Corneal specialist's calm manner and clear explanations.
However, the first specialist still wants to inject the eye with antibiotic because of the health risks in case it is a bacterial infection. I stay with Ed to support him as 'needles in the eye' are his worst nightmare.
The specialist freezes Ed’s eye with two injections of anesthetic, puts a spring opener in to hold back the eye lids, takes samples for culture and injects two small syringes of antibiotics into the two sides of the eyeball. He removes the spring which ‘snaps’ over the eye as it is removed. A temporary shield is put over the eye.
We are told to continue with the Prednisolone and Vigamox every 2 hours and to see the Corneal specialist again tomorrow. Ed actually feels much better as his eye is frozen but, unfortunately, his terrible acid, burning pain returns in a few hours when the freezing comes out. Ed is in discomfort all of the time and also feels a ‘scratching’ on the inside of the eyelid.
July 12, Wednesday – We see the Corneal specialist. The ‘glue’ has held, he says, but the contact lens has broken into two pieces and he has to ‘fish’ them out, which he does. I say that I think this lens might have broken when the first specialist took the spring holder out of Ed’s eye after the antibiotic injections. The Corneal specialist agrees this might be so.
The Corneal specialist says that the cultures from Ed’s eye must be identified and Ed's eye 'calm' with reduced inflammation before a corneal graft can be done. He will call us if anything unusual on the cultures comes back. For now, he puts Ed on an oral, once a day antibiotic, Moxifloxacin, and asks that we continue the Vigamox and Prednisolone every 2 hours. He puts another contact lens on Ed's eye for comfort. However, this lens comes out in a few hours. I see it later lying on Ed's cheek (It is a soft, blue, plastic contact). Ed can still use the Cyclogel for comfort. Ed is taking Tylenol extra strength every 4 hours to try and control level 3 & 4 pain.
We are relieved to being seeing specialists but Ed's pain is making him weak. I'm emotionally distressed. We keep the house window blinds closed and put blankets up to keep the house in darkness. Ed's sensitivity to light is severe. When we go outside, he must keep his eyes closed and wear his dark sunglasses as well as a band of dark cloth around his eyes. And a hat.
July 14, Friday – The Corneal specialist phones us in the morning.
There is a fungus growing on Ed’s eye cultures. The specialist wants us to start special anti-fungal eye drops today. They can only be made in the city. Ed’s daughter arranges to have the eye drops flown over by float plane, and we begin the drops at 6:30 pm.
These special Voriconazole anti-fungal eye drops are to be give every hour when Ed is awake, except between midnight and 6 am. The Prednisolone and Cyclogel are to be stopped. Vigamox drops (antibiotic) to be given every 2 hours. Ed feels an immediate drop in pain to a level ‘1’after the first Voriconazole drops are given the first few times, but then his pain returns to a level 3. Ed keeps taking Tylenol. We are relieved to finally have a diagnosis. I look up the fungus and its treatment on the Web.
Ed's eye culture samples grew Aspergellis fungus. The Aspergellis spores are everywhere and particularly in the soil and on plant material.
But, it is rare for Aspergellis to grow on and inside of the eye. Ed's infection seems to be a 'freak' result after cataract surgery.
July 15 – 3 am, Saturday. Ed wakes up with the same ‘shooting’ pains in eye and a headache over the eye. Level 5 pain. He takes 1 Advil. We continue the new Voriconazole drops early at 4 am. By 10 am, Ed is feeling better than he has for days. His pain is only 1 or 2. The headache and shooting pains are mostly gone. His eyeball feels bruised and is aching, and he still has extreme light sensitivity.
July 16, Sunday – I continue to give Ed the hourly drop of Voriconazol, Vigamox every 2 hours and the oral Moxifloxacin daily. Ed's symptoms are eye aching, stomach queasiness, fatigue, tearing clear fluid with some crusting, but only a few shooting eye pains and infrequent slight headache.
His pain level staying around 3. He has ‘shuddering’ at times in his body when the 'shooting eye pain' happens. He finds that taking one Advil together with one Tylenol gives the best pain relief.
Sunday, 6:30 pm - Ed has only 0.5 level of pain which is the lowest level that he has had for weeks. Later, the pain creeps back up to 2 or 3 so he stays on one Tylenol plain 325 mg. and one Advil 200 mgm., every 3 hours.
He can't take any Codeine as it upsets his stomach.
July 17, Monday – Ed is examined by the Corneal specialist. Eye pressure is normal at 19. Because of Ed's pain, the specialist restarts Prednisolone eye drops twice daily and Cyclogel 3 times a day as we need it. He says to STOP Tylenol because it is too hard on the liver, and to use Advil 400 – 600 mg up to 4 times a day for pain. That means he can have 2 – 3 200 mg. tablets of Advil (ibuprofen) up to four times each day. Every eye exam hurts Ed because of his light sensitivity.
The specialist says that the cultures from Ed's eye show that the fungus is growing on the cornea and also inside the anterior chamber of the eye.
The Corneal specialist wants Ed to start taking oral Voraconazol and to see the infection control specialist at the main hospital who will monitor the effects of this fairly new and powerful anti-fungal drug.
The Corneal specialist also sends us to the Eye Center again, this time for Ed to be examined by a Vitreous & Retina Specialist.
Same day: 5 pm. The Vitreous and Retina specialist examines the Posterior chamber of Ed's eye and the retina which appears to not be invaded yet by the fungus, although he can't be sure. This specialist looks up several research studies on Websites through the University's library and decides on the best treatment to kill the fungus. He explains what he is doing and lets us watch. We like his approach and feel confident in him. He decides that Ed should have an injection into his eye of either Voriconazole or Amphotericin B.
The Vitreous and Retina specialist is kind but also direct with us. He says that this fungus infection could cause Ed to lose his eye. This news is shocking to us. Ed and I cry a bit but then we gather our strength to move on. We are impressed and comforted by the specialist's openess, quickness and intelligence.
Same day-7:40 pm. Ed's eye is injected with Amphotericin B by 2 doctors who are opthamologists training to be specialists. No freezing is used except numbing drops because, this time, it is only a small amount to be injected. However, the injection is very painful. Ed is brave and I am not.
Ed's eye pressure reduces to 12 once a second needle is used to withdraw some fluid from the eye.
Ed has been in a lot of pain all day, but the large doses of Advil are helping.
Same day - 8pm. The first dose of oral Voraconazole is given. It is an expensive drug and the hospital gives us 2 more pills to last us until tomorrow. We must get more oral Voraconazole from a pharmacy. Ed must take 2 Voraconazole pills each day, 12 hours apart.
9pm. Ed is able to sleep better this night.
July 18 – We pick up oral Voriconazole prescription. It costs $700 for 14 pills. Wow! We don’t have our drug card with us, so we have to put the full amount on Visa. We will get 80% refunded by Ed’s pension health insurance. The government doesn’t cover this drug yet.
Same day - 1:45 pm. We see the Infectious Disease specialist (who looks and acts like Ed's son and makes us laugh, which we really need. He is also very kind.) He orders blood tests right away and then every week after that for 2 weeks. We must see him regularly so he can let us know if Ed’s liver can tolerate Voriconazole. Ed is in good spirits and feeling better than he has in a long time. No more body shudders, no stabbing pains and eye ache is only at a level one. We decide it is the result of the Amphotericin B injection from last night and the 2 doses of oral Voriconazole. He still has extreme light sensitivity, and I lead him around everywhere with both his eyes closed. He trusts me so much! We keep hydrated and Ed can still eat.
Same day - 3pm. We see the Vitreous and Retina specialist and 3 students who all look at Ed’s eye. The examination light is painful for Ed. The vision in his left eye is only a little improved. The specialist says that the eye itself looks the same with no improvement. He does an ultra sound of the back of the eye (back chamber) and it looks the same as yesterday. His concern is that the fungus will travel to the retina and destroy it and thus any chance of vision. We hear the specialist say that he would just take that whole piece of infected cornea out.
Same day - 3:30pm. We see the Corneal specialist. He thinks about the situation a bit. I look over the specialist's shoulder and see that the fungus 'clutch' seems to have slid lower down over Ed's pupil in his eye. I wonder if it is dissolving?
The Corneal specialist decides to book surgery for the next day.
The specialist explains that he will remove the diseased portion of the cornea and then sew on a corneal ‘patch’ (a piece of donor tissue).
He tells us that, during the operation, he will also remove the infected fluid from the Anterior chamber (it will fill up again naturally during the operation) and he will ‘flush’ the whole area with more Amphotericin B. This sounds like a ‘full guns’ approach and we are happy that he is being aggressive. This surgery will be done under a general anaesthetic because it takes a longer time and there must be no movement of the eye. Ed is very pleased with this announcement.
We go to a nearby hotel (booked for us by Ed's daughter). Ed eats late as he must ‘fast’ in the morning. He is very tired and still in pain and taking lots of ibuprofen (Advil). And, of course, he gets eye drops every hour from me. We get into our routine, rest, and hope and pray that the ‘nightmare’ will soon be over.
July 19, Wednesday – 9am. We walk the 2 blocks to the Eye Care Centre to see the Corneal specialist once more before surgery. He is delayed in traffic. Ed is ‘shaky’ from fasting so we get permission for him to drink sweetened clear fluids. I buy Gatorade right on the floor we are on, from a little counter there. I don't like to leave him alone very long as he is in pain and cannot see very well due to light sensitivity. It is very bright in the Eye Care Centre. The architect has put in many sky lights. Maybe a good thing for poor eyesight but a very bad thing for light sensitivity.
First we see a specialist 'in training', who removes a piece of tiny plastic from Ed's eye that is part of the gluing which has finally not held.
The Corneal specialist arrives and says that the cornea has sealed itself over, so far, but Ed needs to have the cornea repaired today as it is thin and fragile. He says that there is a risk of hemorrhage and damage to the eye during surgery.
There is also the risk that the contents of the anterior chamber will ‘burst’ through the fragile sealed ‘hole’ area of the cornea if surgery is delayed.
Ed must 'fast' now, even from fluids as the general anaesthetic requires 4 to 6 hours of nothing in the stomach. We walk slowly back to the hotel and wait for the call to let us know what time to go to the Hospital where the surgery will be performed.
We get the call at 11 am and are told to arrive at 1:30 pm. We are there at
1 pm. Ed’s surgery is booked as an Emergency Outpatient surgery and even the admitting clerk doesn’t know we are coming! Good thing the nurse knew, or we would have ended up being sent to a different entrance, and we would have probably lost our cool!
Ed gets all set up in a bed with a night gown and all questions answered.
The anesthetist comes and starts an IV to make sure Ed is hydrated (now it is 3pm) but says that Ed seems quite hydrated (he can tell by how the IV goes in). I say, that’s due to the Gatorade! The nurses and everyone are excellent and so kind. Ed is making jokes and we spend a nice hour together being calm and loving with each other. I’m not afraid because anesthetic is quite safe (safer than flying!) and I’m so happy that the ugly fungus will be cut away and the pain will be gone!!!!! Ed is rolled into the OR saying, “love you to eternity and beyond.” He means "to infinity and beyond" (from Buzz Lightyear). I go for a walk to get food for later. I’m relieved and exhausted.
Same day - 6pm. I happen to see the Corneal specialist as he is leaving. The operation went well, he says. He says that Ed is ‘confused’ and is still 'coming out 'of the anaesthetic, but he thinks Ed will be able to go back to the hotel with me tonight.
Same day - 8pm. Ed is brought to the 4th floor of the hospital. I am told that the doctor has decided that Ed will stay overnight in the hospital.
Ed had to be sedated in the recovery room because he was agitated while gaining consciousness. Ed is drowsy but smiles at me. (He remembers making noise in the Recovery Room but not able to stop himself).
I take over his care and the nurses let me do his drops (after a nurse takes the protective eye shield off the first time for me, because I’m nervous).
Ed is still on the Voriconazole drops every hour (except overnight) and Prednisolone and the same antibiotic drop. I’m OK because his eye doesn’t look any worse than with the fungus. Ed is not in pain, just drowsy. He gets ice chips and gets comfy and goes to sleep. It is very warm in this old hospital, but the window actually opens and there is a great view of trees and homes and it is remarkably quiet.
I stay with Ed all night, making him comfortable. At one point, I lay down on the floor on blankets beside him and sleep there for an hour. It’s not too bad!
July 20 - 5am. We leave the hospital before all the hustle and bustle and get back to the hotel in the cool dawn to avoid the direct sun. Ed’s eye is still light sensitive, and he tires quickly. He has no more burning, only an eye ache. I buy milk and he has porridge in our room. We have a microwave. We decide, with my coaxing, to stay one more night in the hotel. We also decide to take a taxi to the Eye Center (only 2 blocks and it only costs us $5 with the tip!). It’s a bit uphill and Ed is too shaky to walk. The surgery and the anti fungal drug has worn down my strong husband.
Same day - 4pm. We see a specialist in training who measures Ed's eye pressure which is elevated to 30 so he gives Ed a drop of Combigan and gives us the bottle to give one drop twice a day. Now Ed has to have 4 different drops! Good thing I've made a schedule to keep track. Ed is feeling better so we walk very slowly back to the hotel. It is almost pleasant as Ed's pain is greatly reduced. He has to be led, however, the sunlight is way too strong. We stop and rest on a bench after one block and have a cold pop. And more eye drops. Of course.!!!!
July 21 – Friday We leave from our hotel at 5 am. This is the best time to drive through the city to the ferry. Dawn is just breaking and there is little traffic. We get to the ferry in 30 minutes and Ed has an hour sleep in the van before the 7:25 am ferry loads.
Today is a turning point as Ed has zero burning pain in his eye. No pain!!!!! His eye still aches, and he is taking ibruprofen regularly, but it is post surgery pain and not that awful burning pain which he has suffered with for several weeks.
We get home and hide away in our darkened home. The oral Voriconazole (anti fungal drug) is causing Ed to experience visual ‘disturbances’ – namely a ‘white’ screen when his eyes are closed and also some interesting 2 ‘D’ screens, like tapestries of various things; like a green meadow, a countryside, a wolf, a fox, a bumpy, furry blanket, a Chinese warrior. These ‘disturbances' last for about an hour. He enjoys them except for the wolf who appears ferocious. The infectious disease specialist has explained that there would be visual disturbances from this drug and not to drive, etc. However, he didn't mention the movies.
July 22 – Saturday. I send this ‘update’ email to friends and family.
Hi everyone. I finally have time to give you all the update on Ed's eye health! And, thank you for all your positive wishes, thoughts and prayers! We feel your energy and are cautiously optimistic that specialists have made Ed's eye have a good chance to recover.
So, last Wednesday, late afternoon, Ed had an emergency corneal transplant 'patch' surgery done. Ed was given a general anaesthetic much to his relief. During the operation, the surgeon also removed the fungus 'clutch' seen on the cornea as well as taking out fluid from the anterior chamber of the eye, as this fluid was also infected with the fungus. The fluid is replaced by the body within minutes. The surgeon also 'washed' the area with a powerful anti-fungal drug (Amphoceterin 'B').
This surgery, besides saving the cornea, has also helped Ed so much because the burning pain (acid feeling) in his eye is now gone. He has felt this burning for almost 7 weeks (it is caused by the fungus toxins, I think, and the 'hole' in his cornea). The chronic pain has used up energy.
Ed requires hourly eye drops and other eye drops 4 times a day. I have a great method of 'keeping track', and I'm actually 'joyful' because Ed is not in pain for the first time in weeks. He is still extremely sensitive to light, so we are in our darkened house with sheets and towels up stapled over the windows and the fans on.
This is one of the hottest days of the year! I sit here typing with my feet on an ice pak!
Because of this ordeal, we are increasingly grateful for so many things! Electricity and medical care. Transportation. A feeling of safety. The 'simple' things that so many people in the world do without. We are humbled by this.
We must venture out on Tuesday for blood tests for Ed. The effects of the anti-fungal drug must be monitored through blood tests. The infectious disease specialist will be following these results and we go back to see him in 2 weeks. This Wednesday, we go back to the Corneal specialist.
The future looks promising. Of course, right now, Ed's vision in the left eye is poor. However, since the retinal area was not damaged, the doctors' feel that vision will return to some level, and hopefully, a functional level.
Ed's right eye's vision is fine. However, until the light sensitivity reduces, he can't drive or do much away from home on his own. And, of course, he needs to put in at least 2 weeks of limited activity to give the corneal graft patch a chance to heal. He's got audio tapes from the library to listen to and can read for short periods.
July 23 – Sunday. This day, Ed has taken only 2 ibuprofen for discomfort. He is thrilled to be free from pain. He is still easily tired and has naps.
The oral Voriconazole continues to make the white screen for about 30 minutes after it takes effect. Also, he notices some errors now in identifying colors.
As I peer into his eye every hour to give the drops, I see that his iris is clearing, but I see some yellow deep inside and get fearful. However, his good eye also has these yellow colors, so it’s probably just his eye color.
I don’t think that fungus has a chance against the Voriconazole. Not a chance.
July 24 – Monday. Today, Ed has
NO pain at all...for the first time in almost 2 months! He's been through alot, but, like Ed, he is quickly bouncing back!! My job is to keep reminding him that it is only 5 days after his operation.
We can finally open some drapes and let some natural light inside. Ed's sensitivity to light is also much reduced. He's walking around inside without sunglasses on. Of course, going outside still causes discomfort. We go to his local doctor tomorrow and to the lab (the infectious disease doctor is monitoring how the anti-fungal drug is affecting Ed's liver by checking Ed's blood results every week).
So, no pain, BUT, I can still see some yellow spots around his iris in one place, (under the cornea) so I'm only still cautiously optimistic until we see the Corneal specialist this Wednesday, and he can tell us what those are! I'll let you know. Ed is still on 4 types of eye drops - one kind is every hour except between 12 and 6am. Plus his super potent anti fungal pill twice a day.
July 26,2006 – Wednesday. We saw the Corneal specialist and the graft on Ed's cornea is healing. Today, Ed has his 'old' energy back and he is a happy man! He has to have hourly drops, still, and take the anti -fungal super drug for a number of weeks yet. How much vision returns to the eye will only be known as the months pass.
However, all the burning pain and ache is gone. It feels like a miracle to us. In 3 more weeks, he can resume his usual physical activities of building, chopping wood, gardening etc. This time, however, he'll be wearing a good face shield!!!
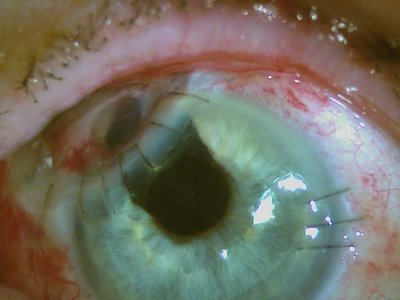
The Corneal specialist sent our e-mail a photo of Ed's eye.
The specialist took the photo for his records and sent it to our email! Even the specialist had to chuckle when he saw Ed's eye, because it looks like there are two pupils. The specialist explained that so much of the sclera was infected and had to be removed that it has left a hole under the new corneal patch which shows up as black. He is hoping that it will scar over and be a white colour in time. This eye surgeon specialist is amazing and we are so grateful to him.
July 29, 2006. Ed is still feeling much better although he tires easily. He can now be without his dark sunglasses on when in the house, even with the blinds open. He can read and watch TV again, using his good, right eye. The left eye's vision is still poor. We wait and see. We'll see the Corneal specialist again this week.